Fee-for-service primary care creates a strange paradox: clinics earn more when patients return sicker. Rethinking this model isn’t just philosophy, it is a data architecture problem.
All over the world, primary care is often structured in a fee-for-service model. That is, when a patient arrives with a problem, a doctor treats that narrow issue, and the provider is paid for each service delivered. In this model, the number of visits or services is incentivized, and not comprehensive patient health.
In these fragmented primary care environments, clinicians usually don’t have access to complete patient histories, nor do they need them. Preventive care, early intervention opportunities, and long-term health outcomes are generally out of scope for a visit. India’s healthcare system is much the same.
Clinikk, a health startup based out of Bangalore, set out to fix this model.

Changing primary care incentives
Clinikk built a subscription-based model where patients pay an affordable, fixed monthly fee and all outpatient services are covered. This includes unlimited consultations, lab tests and medication. With this model, they flip the incentives in traditional primary care. Clinikk only succeeds when patients stay healthy, and so it becomes necessary to avoid complications and prevent avoidable hospital visits.
This model then has different requirements for delivering care:
- Clinicians need access to comprehensive patient history in every visit
- Clinical workflows, documentation and protocols must be repeatable
- Every clinic that’s part of the network needs to provide consistent, and continuous care
- Identifying preventive care and early intervention opportunities must be systematic
To make this possible, Clinikk needed technology that could support long-term clinical needs, and not only record information about a single encounter. This meant storing structured vitals, labs, diagnoses and treatment plans in a way that could be retrieved and analysed over time.
Why existing EHR systems fell short
Most outpatient EHRs available in the market catered to the fee for service model. They focused on capturing encounter details, generating prescriptions and recording billing information. They were not designed to store years of structured clinical information, identify trends or support preventive and protocol driven care.
For example, most systems store clinical notes as free text or semi-structured templates, making it difficult to build dashboards, conduct protocol checks or trigger CDS rules.
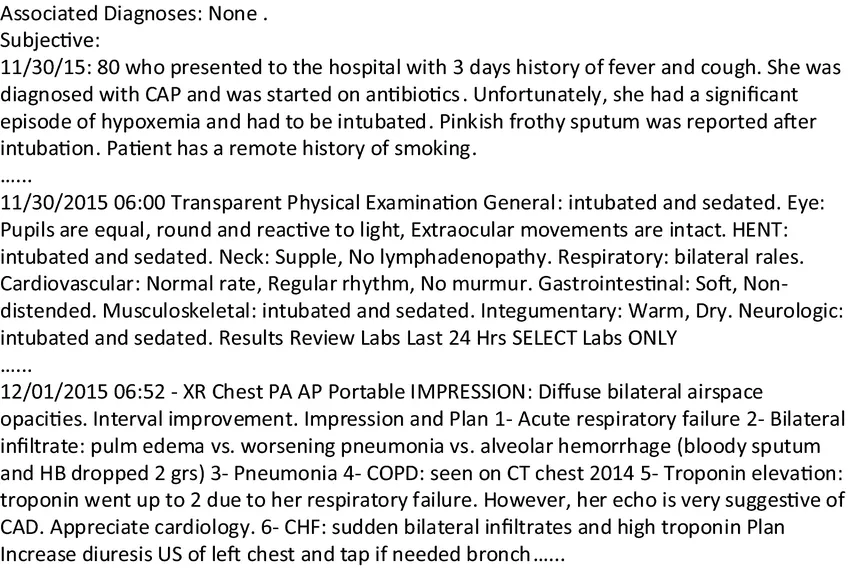
This type of system also reinforced care fragmentation in the type of patient data it was able to record and analyze. In most cases, it is difficult to compile and report comprehensive, longitudinal data about a patient from various sources. Even when APIs are available, they are encounter-centric, returning flat snapshots that do not contain the semantic structure needed for trend analyses.
Clinikk’s software needs were fundamentally different, they needed a system that could,
- Store longitudinal health records
- Handle evolving care protocols and workflows
- Integrate clinical decision support
- Enable consistent care across health centers
And so, they decided to build what didn’t exist, and partnered with Medblocks to do it.
Designing for long-term health
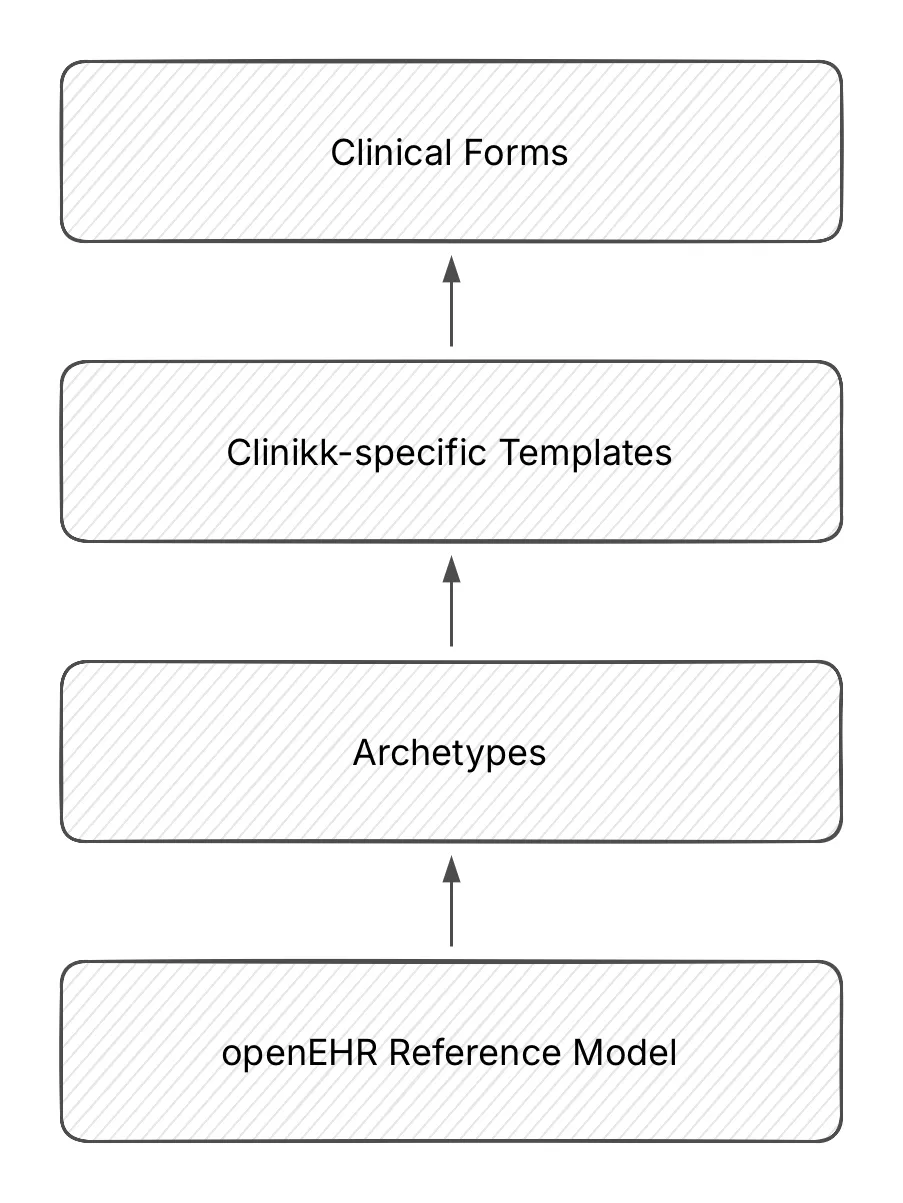
Medblocks worked closely with Clinikk’s product team and clinicians to translate real world workflows into software. This was through spending time in clinics, understanding clinician workflows and iterating quickly based on feedback. The workflow was prototyped through openEHR templates, allowing both teams to modify form structures without interacting with database schemas.
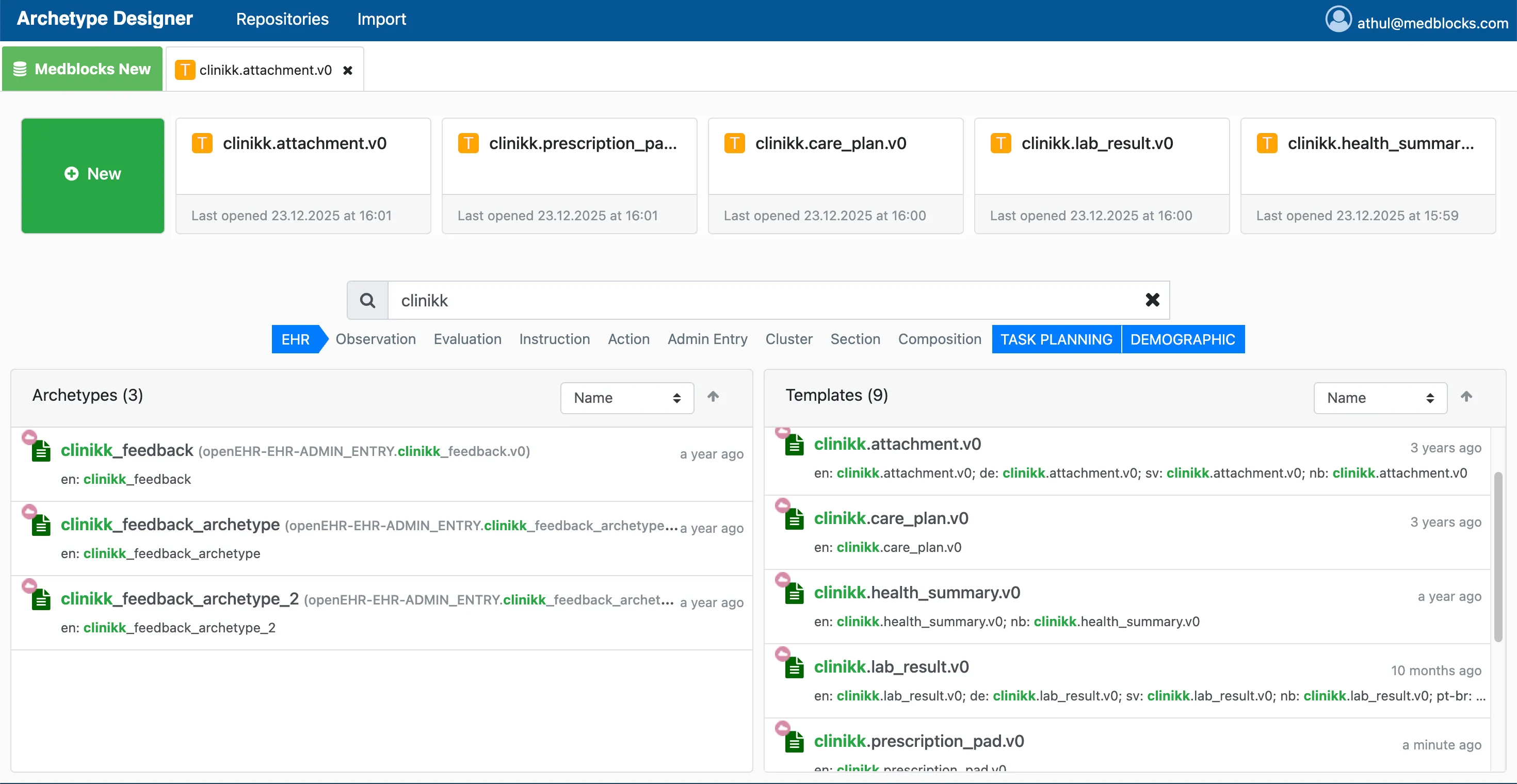
At the core of the system is an openEHR-based data layer that formed the system of record. This allowed Clinikk to,
- Store structured patient data over years
- Use existing openEHR archetypes for clinical concepts
- Add new data over time without redesigning the database
- Build new clinical workflows over the same data model.

Three main advantages of using openEHR emerged:
- Clinical meaning was separated from the underlying data model, and so the system was flexible
- The maximal modelling approach allowed extensibility of features and data types
- Existing data models built by the openEHR community could be reused and combined into templates
- New templates could be added for new applications without changing the data schema used in existing applications
Clinical impact for doctors
The impact was immediate for doctors. The new platform was designed to support their patient interactions, and convey information effectively. Clinicians reported smoother workflows, greater confidence in decision-making and that they felt supported by the system to deliver necessary care.
Clinical dashboard that reduced cognitive load
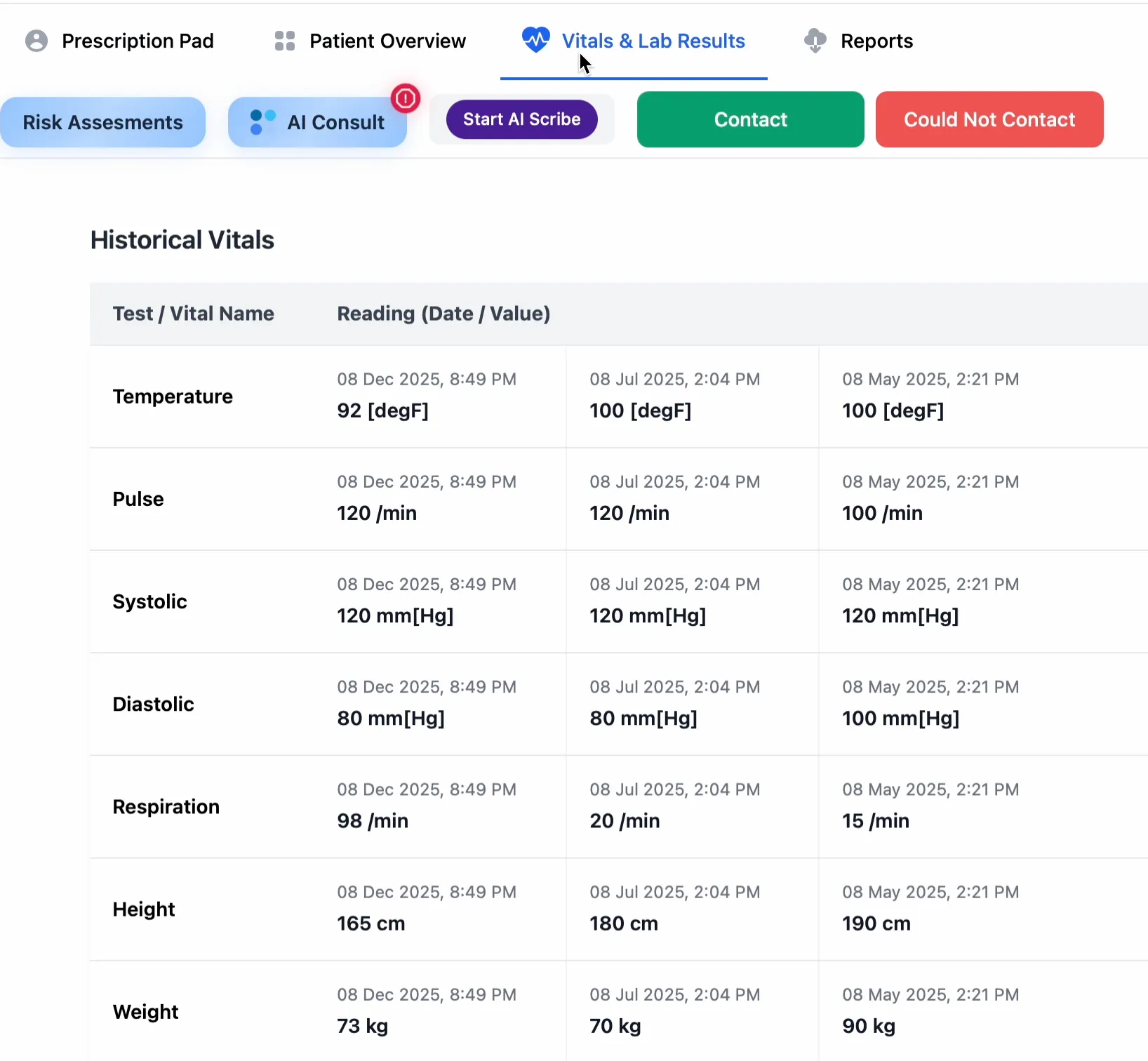
The new clinical dashboard was designed to reduce cognitive load and depict all relevant patient information in one place. With this, doctors no longer needed to scroll extensively or navigate slow-loading pages. It also became easier to customize views and fields based on the patient or situation. The dashboard was built in a shared React App, and co-built by Medblocks and Clinikk developers. Medblocks also supported writing AQL queries and pre-defining templates and variables.
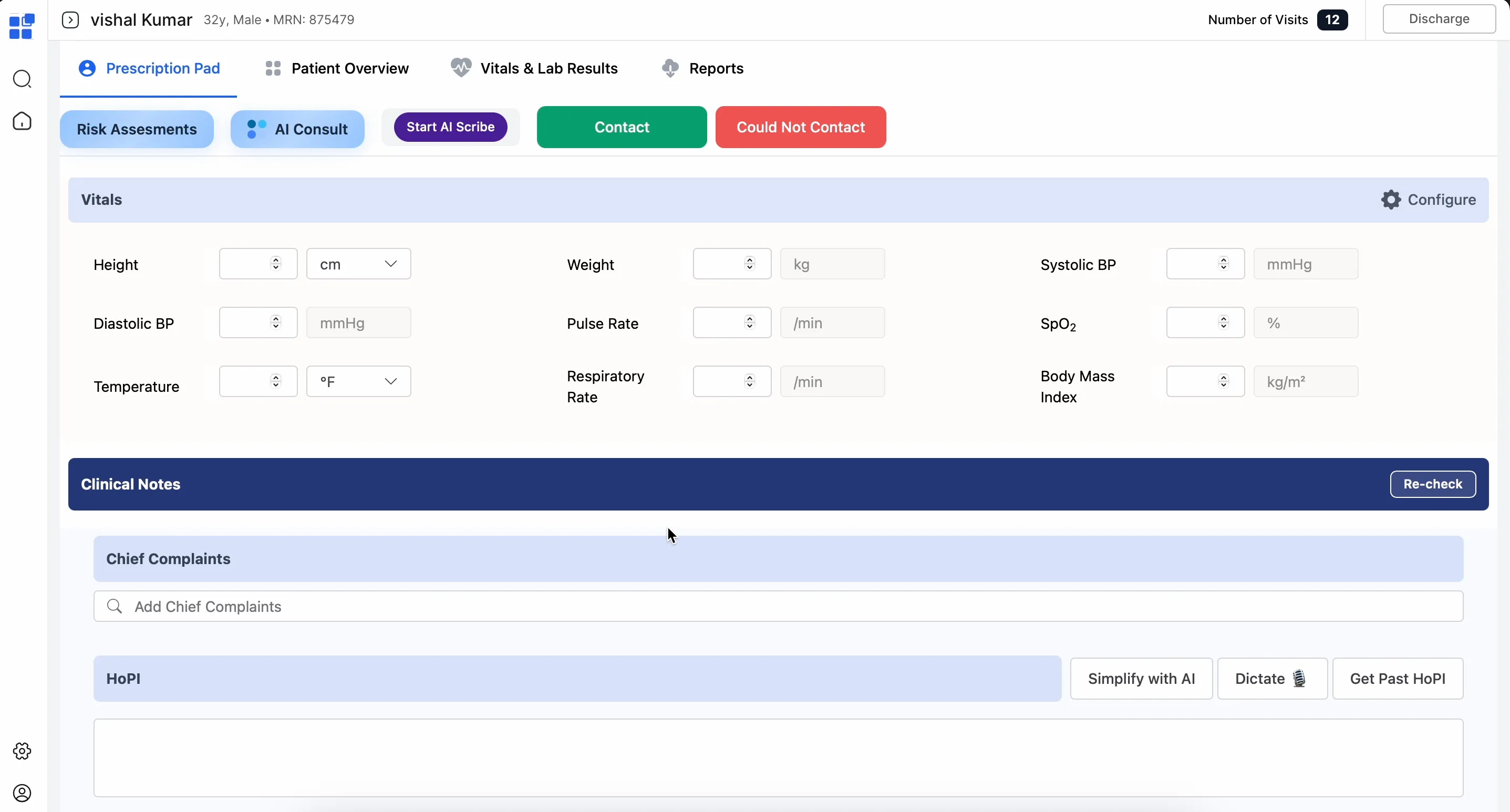
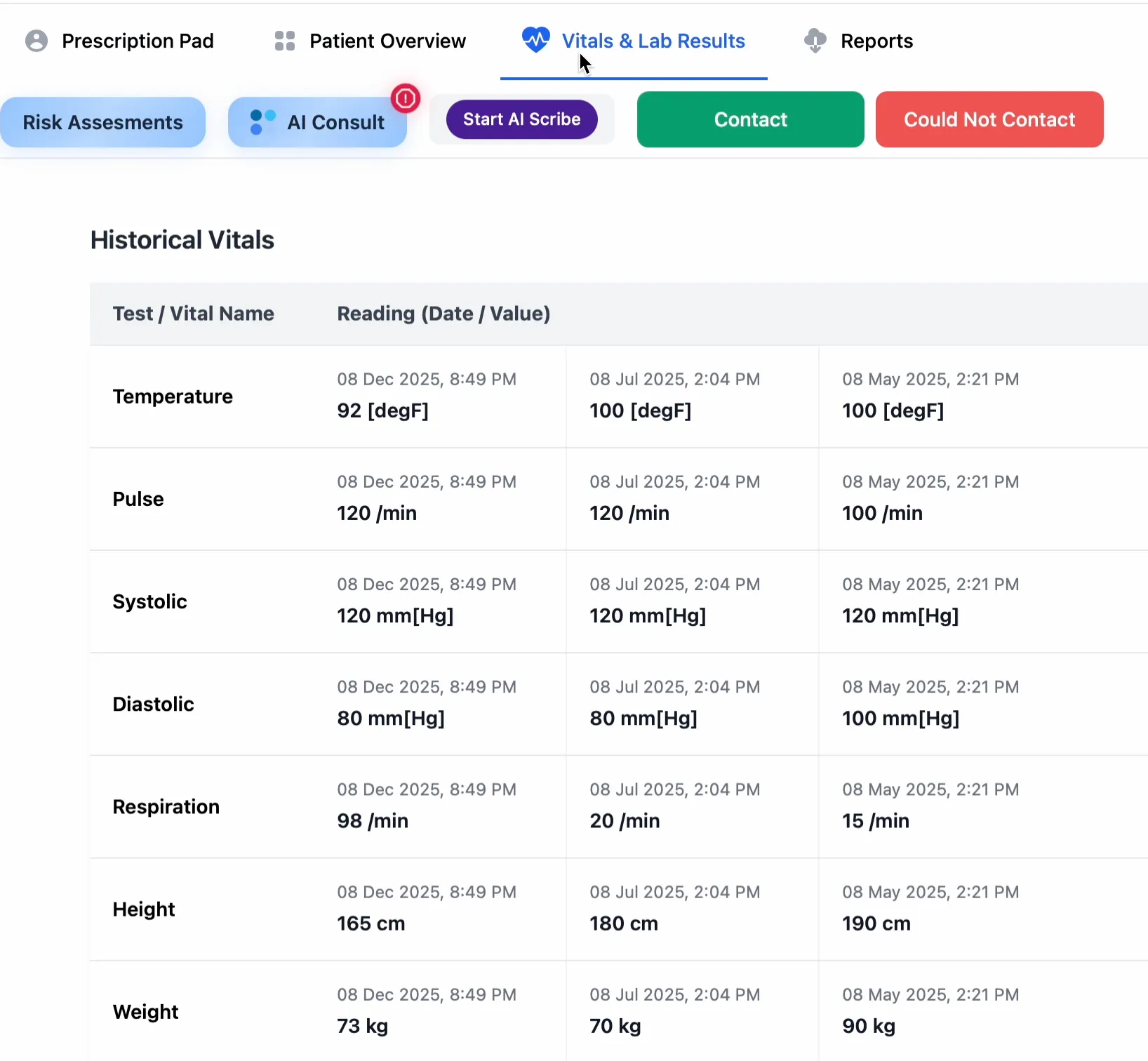
Longitudinal data insights
Having years of clinical data available instantly changed how care was delivered. Clinicians could now see trends across time and communicate them easily with patients. These views relied on time-series extraction of compositions from the openEHR Clinical Data Repository, and were plotted directly from structured entities rather than processing free-text.
To make this possible across Clinikk’s Health Hubs, clinical concepts were standardized using SNOMED-CT and handled at the data layer. openEHR’s CODED_TEXT allowed multiple terminologies to be represented when needed. For medications, a pharmacy-specific list was used which also integrated with the inventory management system to show stock availability. This was also stored as coded values in openEHR, allowing consistent longitudinal views, trend analysis, and cross-center comparisons.
It became easier to monitor the progression of chronic diseases like diabetes and hypertension, and identify opportunities for early interventions. And, because all centers operated on a single shared data platform, a patient’s history was available at every Clinikk Health Hub.
Accessible protocol-driven care
One of the most impactful improvements made over time, was to surface treatment protocols during a clinical encounter. When a doctor entered a diagnosis, relevant order sets and treatment guidance appeared instantly. This helped clinicians make decisions faster, improved confidence, and ensured consistency across clinics.
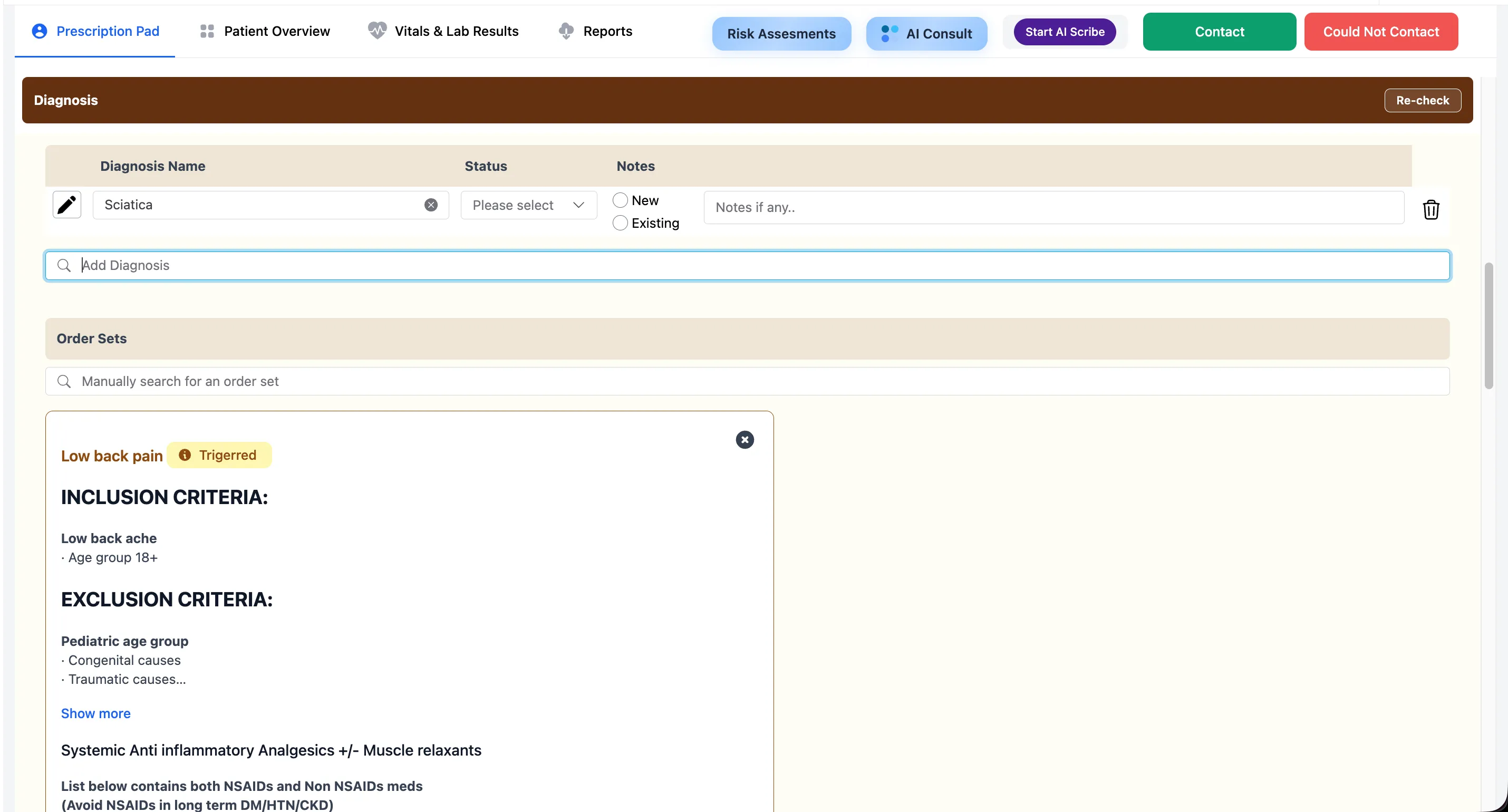
Protocols were authored and managed in Directus, acting as a lightweight clinical knowledge Content Management System (CMS). Clinicians could define treatment protocols in simple, structured data models defined in Directus. Treatment protocols included mapping diagnoses to recommended investigations, medications, follow-up intervals and so on.
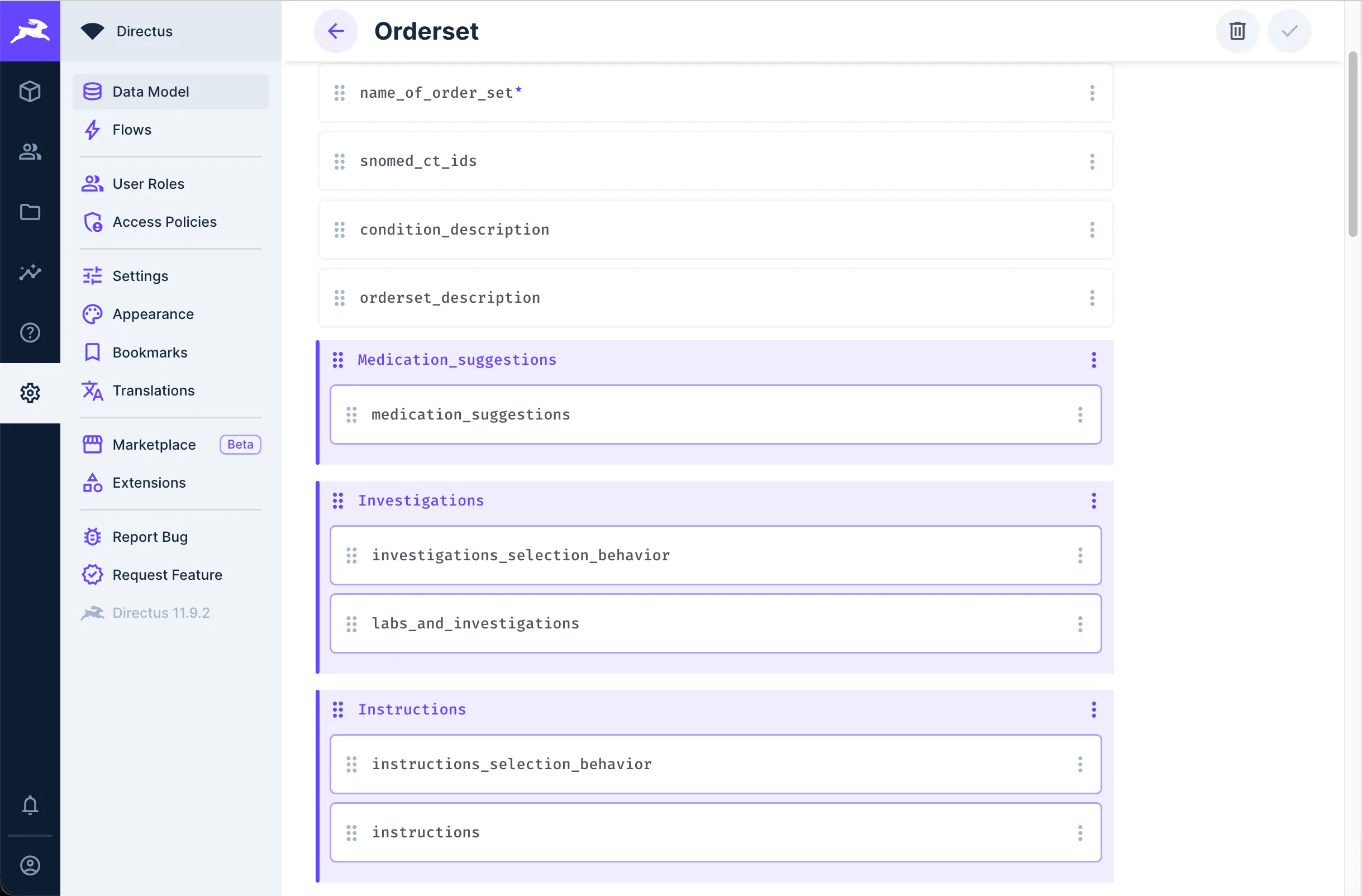
These structured protocol definitions were dynamically consumed by the React-based clinical application at runtime. This architecture allowed protocols to be updated, refined and expanded without redeploying the core application.
This also allowed easier monitoring of protocol adherence and deviations. When a clinician chose to override or deviate from a recommended protocol, that decision and rationale was stored back into the openEHR CDR using a custom archetype. This ensured that protocol execution remained part of the clinical record, and enabled auditability, learning and future improvement.
Simplifying everyday tasks
Beyond supporting protocol driven workflows, the platform also simplified everyday tasks like finding and prescribing medications. Through integrations, it showed doctors the availability of stock while prescribing medication and listed the lab tests available with the partnered laboratory service.
Tech built through deep collaboration
Medblocks and Clinikk worked closely to build this platform, with direct input from Clinikk’s doctors to understand their workflows. Medblocks built the underlying data model, ensuring a scalable and standard-based structure. This also included how information was modelled and how the patient record would accommodate change over time.
This let Clinikk’s development team focus on the clinical design. There was a tight feedback loop between clinicians, in-house developers and the Medblocks team, allowing the platform to grow quickly and adapt to new requirements. Clinical form changes were handled through updating openEHR templates, without changing the underlying data model. Clinical protocol changes, on the other hand, were managed through content updates in Directus, rather than requiring code changes. This separation allowed feature updates to be rolled out within days instead of weeks.
This close collaboration also allowed clinicians to be deeply involved in shaping the tool, instead of being restricted by an out of the box solution. Clinicians routinely tested new workflows in a staging environment connected to a parallel openEHR CDR to ensure safety before rolling out features across all hubs.
Wrapping up
Clinikk’s mission to provide subscription-based primary care required more than changed incentives, it needed a solid technical foundation. Conventional EHR solutions didn’t solve for this, instead focusing on documenting isolated encounters and billing. By working closely with Medblocks, Clinikk built a platform that was better suited to support their working model.
This system stored structured longitudinal data and supported consistent, protocol driven care across every Clinikk Health Hub. With openEHR at the core and close collaboration between clinicians and developers, the platform evolved into a flexible clinician-shaped system that suited their needs. The long-term visibility it provided aligned with Clinikk’s care model as well, where preventing complications and future illnesses is both a clinical priority and a business necessity. Together, Clinikk and Medblocks show how the right technical architecture can make preventive, continuous primary care truly scalable.

