India has the world’s largest tax-payer-funded health insurance scheme, PM-JAY or Pradhan Mantri Jan Arogya Yojana. PM-JAY covers 500 million people in India accounting for 40% of India’s population belonging to the lower economic strata. Each family under the scheme gets around 5,00,000 INR (nearly 6180$) each year for illnesses and surgeries that require overnight admission to a hospital.
The policy document recently released by NHA outlines how they want to transition India from Volume based care to Value-based care.
Here’s the document if you want to read it yourself: Click here to find more
Below is a summary of how NHA intends to make the move:
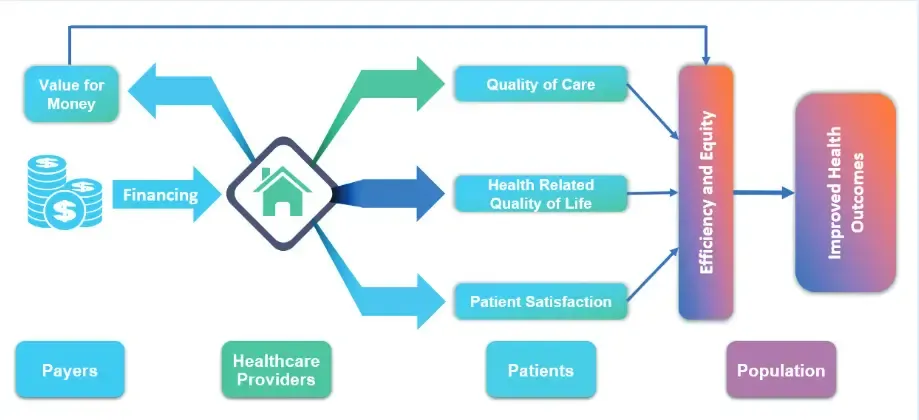 The fundamental goal of the NHA is to increase value for money to the payers and increase overall quality of life. This is measured through two values
The fundamental goal of the NHA is to increase value for money to the payers and increase overall quality of life. This is measured through two values
- Decrease in mortality rates of specific conditions
- HRQoL - Health related quality of life, sometimes called Patient reported outcomes measures (PROMS)
Measuring the first metric is fairly straight forward and can easily be accomplished through simple monthly reports. The latter is a more complex metric to analyze and derive value out of it.
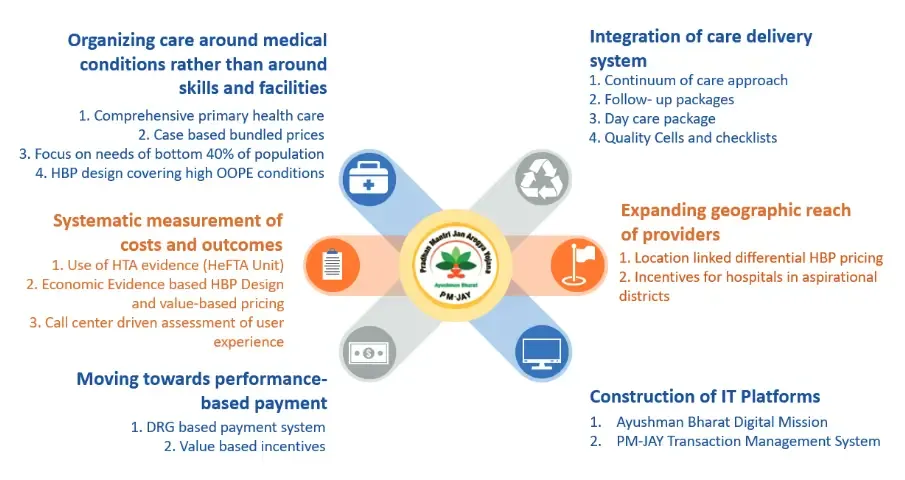
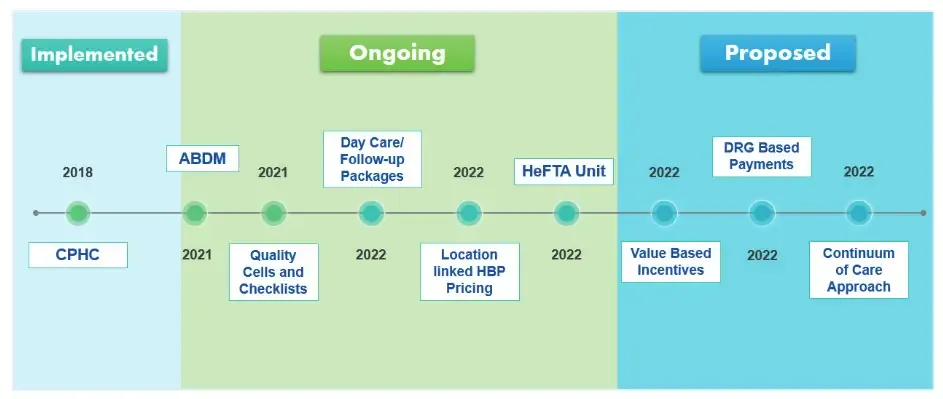
A framework has been proposed to make the shift from volume based care to value based care, here are its brief details:
- Implementing Case-based Bundled Pricing where providers are paid fixed rate for a set of services as defined by a package.
- Starting Health Financing and Technology Assessment which ensure that payment terms and plans are providing best value for money
- Diagnosis Related Group based payment system where payment is linked to the severity, complications or comorbidity level of the case.
- Vertical integration of care delivery systems where new centers are established which perform primary care (extending the existing PHC’s role), refer to higher centers and act as centers for follow-up - for cardiology, vascular surgery and urology.
- Expanding geographical reach where interventions in districts(akin to county) will attract a 10% financial incentive
- Building out a technology platform - implementing ABDM everywhere to make data more accessible for governance and furthering clinical research
 The existing simple fee-for-service system is when doctors diagnose a patient and perform the necessary procedure for which a fee is received. Moving to a value based care system is rather complex and is cross-disciplinary. The responsibility of patient outcome moves from a single clinician/clinician team to the institution as a whole.
The existing simple fee-for-service system is when doctors diagnose a patient and perform the necessary procedure for which a fee is received. Moving to a value based care system is rather complex and is cross-disciplinary. The responsibility of patient outcome moves from a single clinician/clinician team to the institution as a whole.
Incentivizing value based care
The NHA realizes that the existing model of incentive is very flawed and does not work as intended. Hence a new model is necessary - the proposed new model has two parts Certification based incentive and Outcome based incentive.
In fact, in the current design, those hospitals are paid incentives which have registered frauds, denying for treatment, where beneficiaries are charged with out-of-pocket expenses, and where several grievances are raised against accredited/ certified hospitals. It emphasizes that the current design has loopholes, and a new way needs to be explored for ensuring the quality and monitor the value in the healthcare service - NHA document
Certification based incentives are tied to the NABH accreditation grade of the hospital - this accounts for around 50% of the financial incentive. Outcome based incentives are a performance incentive linked to patient outcomes they are:
- Beneficiary Satisfaction Rate
- Hospital Readmission Rate
- Extent of out of pocket expenditure
- Health related quality of life (HRQoL)
- Confirmed Grievances
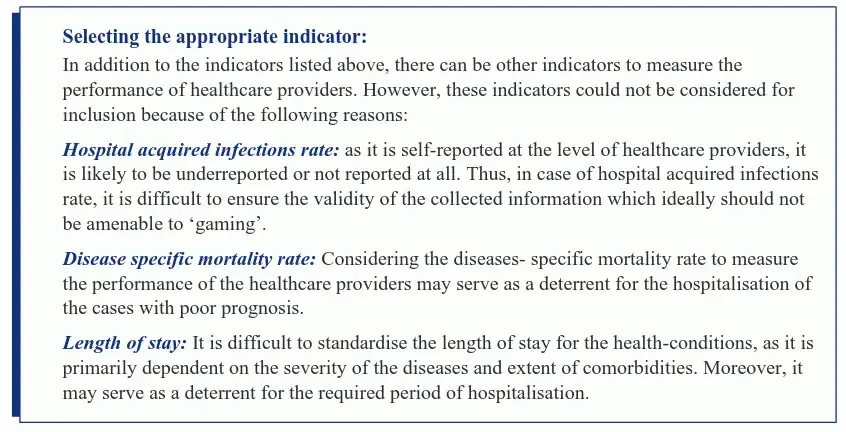 Calculation of outcome based incentives have been outlined in detail in the document. You can download the document directly for further know-how.
Calculation of outcome based incentives have been outlined in detail in the document. You can download the document directly for further know-how.
Role of technology
NHA is already in consultation with NABH to make ABDM compliance mandatory for NABH accreditations. - NHA document
The measurement of outcome based indicators such as hospital readmission rates are really difficult to track - for example, a patient who was operated for appendicitis laparoscopically might present with pain abdomen at a different center. ABDM might make it simpler for centers to onboard new patients seamlessly with complete documentation and history.
For now there is no confirmation on any mandate to implement ABDM in all centers. It seems that it is the next logical step in moving towards value based care.
