Sending data is easy, but making sure it’s understood? That’s where these 4 levels of interoperability come in. In health tech, whether you’re learning, building, or using it, one word that comes up frequently is interoperability, which is the ability of different systems to exchange, understand, and use data seamlessly. But people don’t always mean the same thing by it.
One person’s idea of interoperability might be emailing a PDF, while another imagines real-time clinical decision support across hospitals.
To bring clarity, HIMSS (Healthcare Information and Management Systems Society defined a model with four levels of interoperability. These levels represent how systems exchange data, understand it, and ultimately use it to improve care.
For a quick and clear understanding on why interoperability, here’s a lesson, “Why is Healthcare Interoperability Necessary?”, from our FREE FHIR Fundamentals Course.
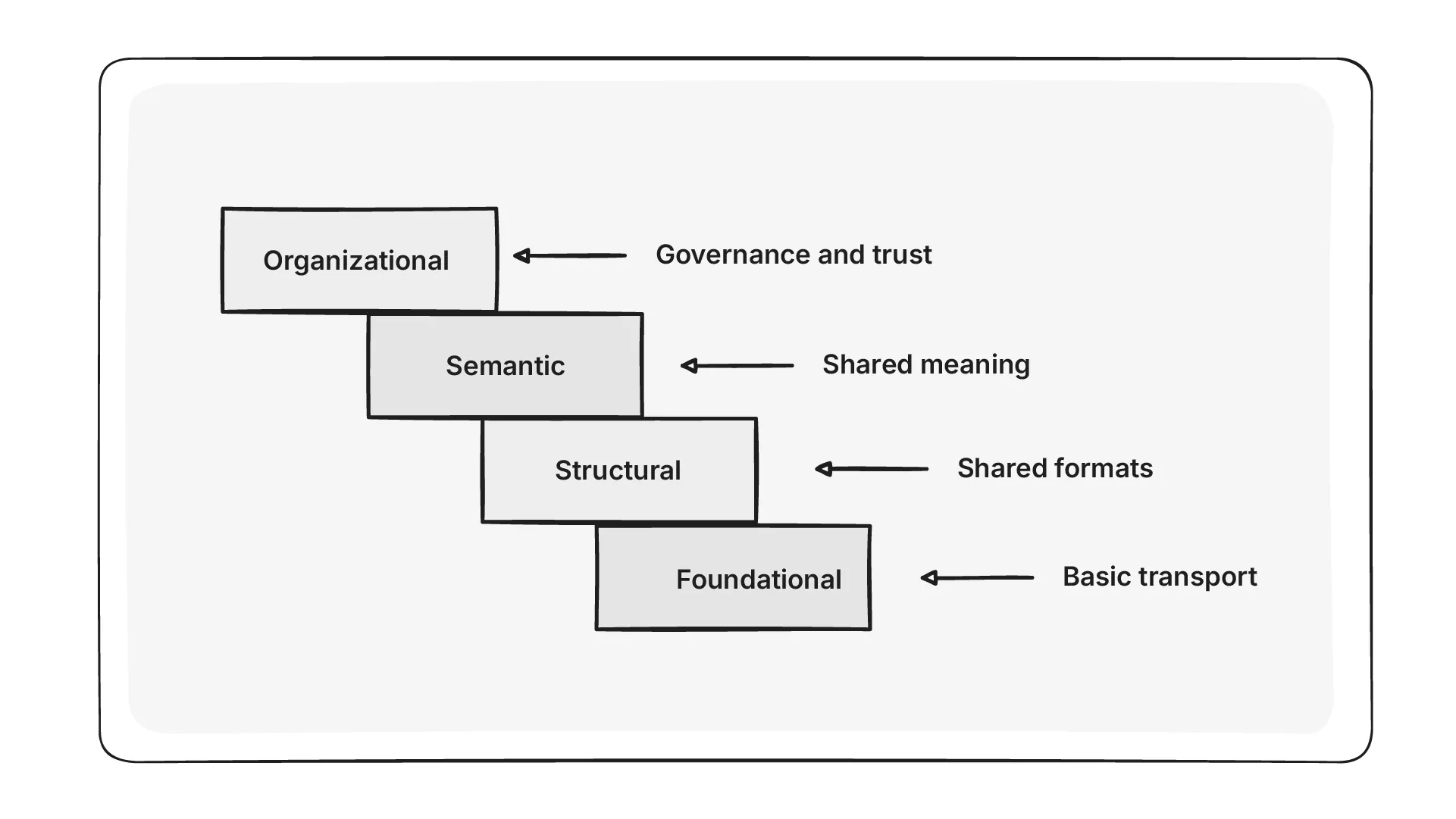
Here are the four levels of interoperability, each showing a different stage of how systems connect and communicate.
Level 1: Foundational interoperability
Basic data exchange, no shared understanding.
At this level, systems can send and receive data, but the information isn’t structured or easy to process. For example, data might come as a scanned document, a PDF, or an email attachment. While the recipient can read it, the data cannot be processed automatically.
Example: A radiology report is sent as a PDF via email. The physician can view the report, but their EHR system cannot extract or store the values for further use.
Level 2: Structural interoperability
Consistent data formats and structure.
This level introduces standard messaging formats such as HL7v2, CDA, or FHIR. These help systems understand the structure of the data being exchanged, making automated processing possible. To learn more about how FHIR enhances data exchange in healthcare, read our article: What is FHIR?
Example: A patient’s lab results are shared via FHIR, and both sender and receiver can process the message format. Still, one system may use different field labels or codes that create ambiguity.
While structured data exchange enables automation, differences in how it’s implemented often mean full interoperability isn’t achieved without manual mapping and intervention.
Level 3: Semantic interoperability
Shared meaning of the data.
At this stage, systems not only understand the structure but also agree on the meaning of the data elements. This is enabled through the use of standard clinical terminologies like SNOMED CT, LOINC, and value sets defined in FHIR Implementation Guides.
Example: Two health systems exchange allergy information using FHIR. Both use the same SNOMED CT codes for penicillin allergies, ensuring the receiving system interprets and stores the data exactly as intended.
At this level, data can be used for accurate decision-making, clinical analytics, and real-time sharing across systems, but achieving it requires investment in standards adoption and careful terminology governance.
Level 4: Organizational interoperability
Collaboration, policy alignment, and real-world use of data.
This level goes beyond technology. It focuses on how organizations actually use shared data. It involves legal agreements, governance models, workflows, and a shared commitment to using data to improve care outcomes.
Example: A hospital, a primary care clinic, and a home health provider participate in a health information exchange. They not only share data but also coordinate patient care based on that shared information that’s supported by common protocols and regulatory alignment.
Reaching this level requires strong leadership, policy frameworks, incentives, and cross-organizational trust. It is where interoperability delivers its true value helping improve outcomes, reduce costs, and enable seamless care delivery.
With the recent CMS (Centers for Medicare & Medicaid Services) rule and guidance from the ONC’s (Office of the National Coordinator for Health Information Technology) roadmap, healthcare organizations must prepare their systems for seamless data exchange.
If you’re still curious and want to learn more, check out our blog, “CMS Interoperability and Patient Access Final Rule” for the full scoop.
Quick recap
Interoperability is about how organizations work and plan together when exchanging healthcare data. By understanding and applying these four levels, organisations can move toward more meaningful data exchange, better care coordination, and improved outcomes. The development of FHIR has helped organizations improve how they exchange healthcare data and coordinate care.
