Why is Healthcare Interoperability Necessary?
Before we dive into the details of FHIR, let’s look at the landscape in which it exists.
The dream of freeing health data from its silos has been discussed for over 3 decades, with numerous standards and initiatives advancing this goal worldwide. The potential benefits would be huge, but so are the challenges that exist.
But what is healthcare interoperability? As defined by HIMSS,
Interoperability is the ability of different information systems, devices and applications to access, exchange, integrate and cooperatively use data in a coordinated manner.
This exchange would extend across organizational and national boundaries, allowing for improvements in the health for individuals and populations.
Some benefits of healthcare interoperability include:
- Improved quality of care for patients
- Reduced physician burden in decision making and coordination with payers
- Enhanced care coordination across stakeholders and departments
- Empowered patients with easily available information about their health
- Public health initiatives supported with greater insights on population health
- Meet regulatory requirements increasingly implemented governments worldwide
Barriers to healthcare interoperability
Here are some of the challenges faced in maintaining interoperable health data today:
- Lack of standardization: Health data is complex and is managed by many stakeholders, including vendors, providers and government organizations. Medical terminology used is not standard, and even when standards exist, adoption and normalization of data to those standards has an impact.
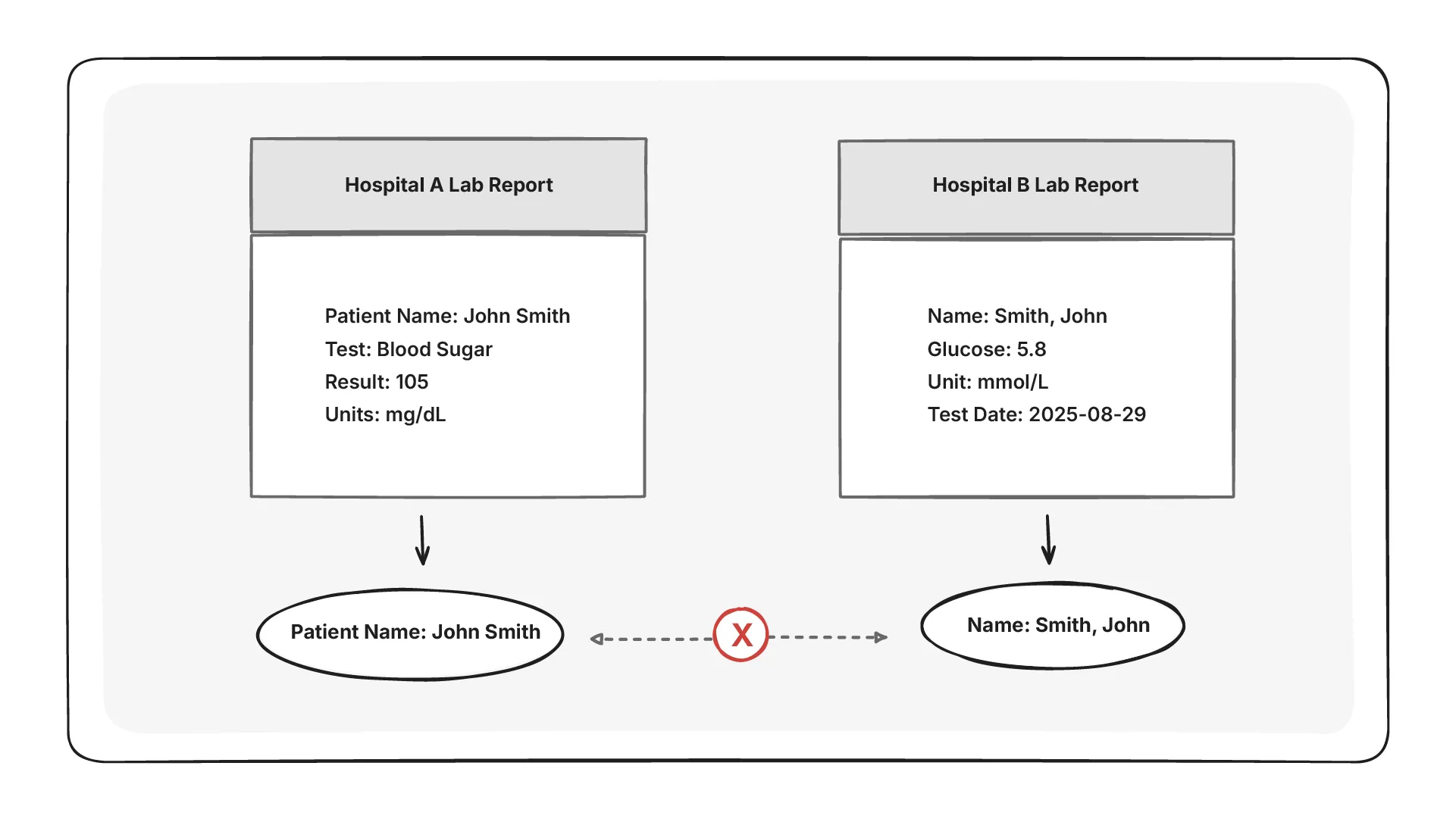
- Fragmented systems and data silos: Currently, a lot of health data exists in silos, even within the same hospital or organization. For example, departments in a hospital may use different and incompatible EHR vendors making interoperability difficult. Standard compliance by vendors is one aspect of this, another is the retrieval of data that is currently in legacy systems.
- Data security and privacy: Sharing health data must always go hand-in-glove with ensuring patient privacy and data security, and can act as a blocker for adopting interoperability standards. In this case, interconnected healthcare systems would reduce the risk of errors and security gaps due to manual intervention.
- Professional burden: Healthcare professionals are often expected to adopt new tools with little involvement in design or selection. EHR systems that prioritize admin and billing workflows over clinical needs disrupt patient care and increase cognitive load. Over time, this mismatch contributes to clinician stress and burn out.
Which of the following is a significant barrier to healthcare interoperability as discussed?
Levels of interoperability in healthcare
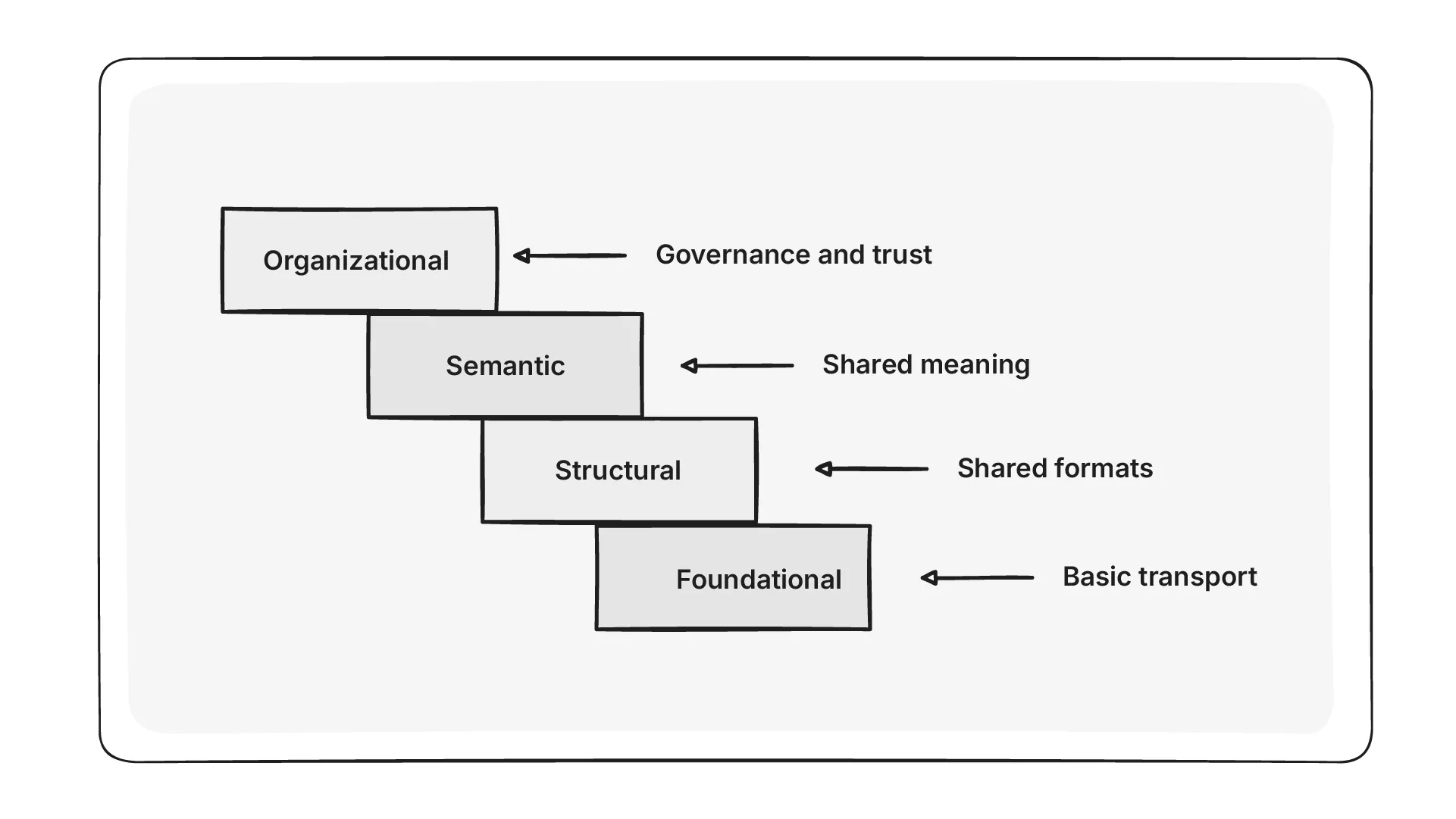
There are 4 levels of interoperability in healthcare as defined by HIMSS and informatics experts. Some of these levels are easier to achieve with existing healthcare IT technology while others require further innovation and development.
-
Level 1 - Foundational interoperability: This is also known as simple transport and is the most basic level of interoperability. Here, data is transferred securely from one device to another, without any transformation or interpretation of data. E.g. APIs to a system.
-
Level 2 - Structural interoperability: This level, also called structured transport, ensures all data is standardized into specific shared formats, making it understandable across different systems or devices. E.g. If two systems use FHIR for information exchange, they are performing structured transport.
-
Level 3 - Semantic interoperability: Semantic interoperability or semantic transport involves exchanging data between systems, such that the receiving system can understand and use the data sent. This would require the systems to use a common vocabulary or shared meaning to represent standardized data. E.g. the HTI-1 rule mandates that crucial data elements in patient care be shared using common vocabulary standards.
-
Level 4 - Organizational interoperability: This level integrates governance, policies, and trust frameworks to enable secure and timely communication and use of data. Initiatives like the Trusted Exchange Framework and Common Agreement (TEFCA) support this, and emphasize the importance of trust, privacy and data governance
Which level of healthcare interoperability ensures that the receiving system can interpret and use the meaning of exchanged data?
Summary
Healthcare interoperability is the key to unlocking patient data from silos and enabling seamless exchange across systems, organizations, and even countries. While the benefits include better care quality, reduced clinician burden, empowered patients, and stronger public health, real challenges remain—ranging from lack of standardization and fragmented systems to privacy concerns and clinician burnout.
The HIMSS framework defines four levels of interoperability: foundational (basic transport), structural (shared formats), semantic (shared meaning), and organizational (governance and trust). Together, they provide a roadmap for building systems that can work together and support better healthcare outcomes worldwide.
