The Nordic openEHR Journey: Interview with Hanna Pohjonen
While many parts of the world are struggling to break health data silos, the Nordic countries have built systems where information flows easily between hospitals, clinics, and social care. This wasn’t driven by regulation or technology, but a culture that believes shared data leads to better care.
Hanna Pohjonen, co-chair of the openEHR Education Program and co-founder of Rosaldo, is a key voice behind Finland’s national digital health initiatives. In this interview, she explains how this culture of collaboration made the Nordic countries a global model for health interoperability. Hanna offers an insider view into the rise of openEHR-driven vendors, the cooperation between FHIR and openEHR communities, and how this has led to sustainable, nationwide interoperability.

Data sharing culture in Nordic countries
“We have always had a very, very strong culture for [data] sharing,” says Hanna Pohjonen, and this culture set the foundation for openEHR adoption in Nordic countries. Cross-organizational patient pathways have long been part of how care is organized, and this led each Nordic country to build national data-sharing infrastructures early on.
Initially, these systems were document-based and relied on formats like CDA and XDS. Hanna notes that these systems helped establish a legal and operational environment to support consistent data exchange across organizations. This early commitment to collaboration and interoperability uniquely positioned the Nordic countries to adopt openEHR at scale.
Why did vendors adopt openEHR?
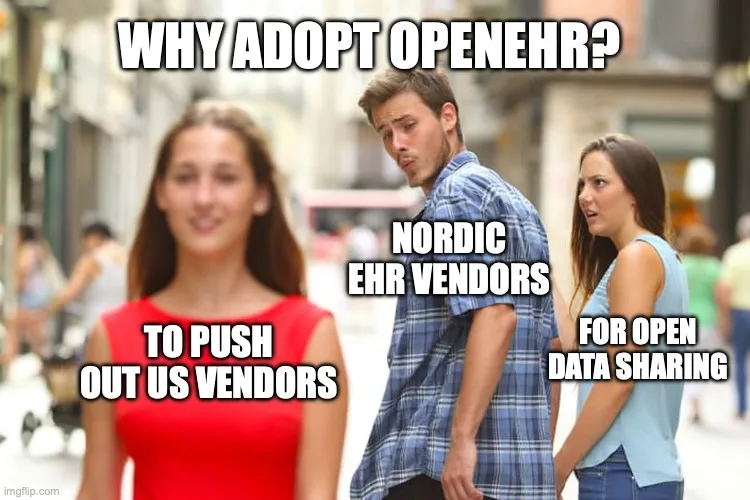
“Our openEHR development has been very much vendor-driven development,” says Hanna, marking a clear difference from how data standards are typically adopted in other countries. When major Nordic EHRs began modernizing their legacy systems using openEHR for their internal data model, their motivation went beyond technology.
Apart from the region’s strong data-sharing culture, this move was also strategic. Hanna explains that the Nordic vendors wanted to differentiate themselves from large US systems such as Epic and Cerner. “They wanted to push US vendors away from the Nordics. This was a key differentiator–that we open up.” The shift towards openness became a shared advantage rather than a point of competition.
Hanna also highlights how rival companies began to collaborate and reuse components, which was possible because of the common foundation in openEHR. This has led to faster innovation, easier development, and co-creation with end users. Key players in this transformation include Cambio in Sweden and Tietoevry in Finland, DIPS and PatientSky in Norway.
Working together with FHIR and OMOP
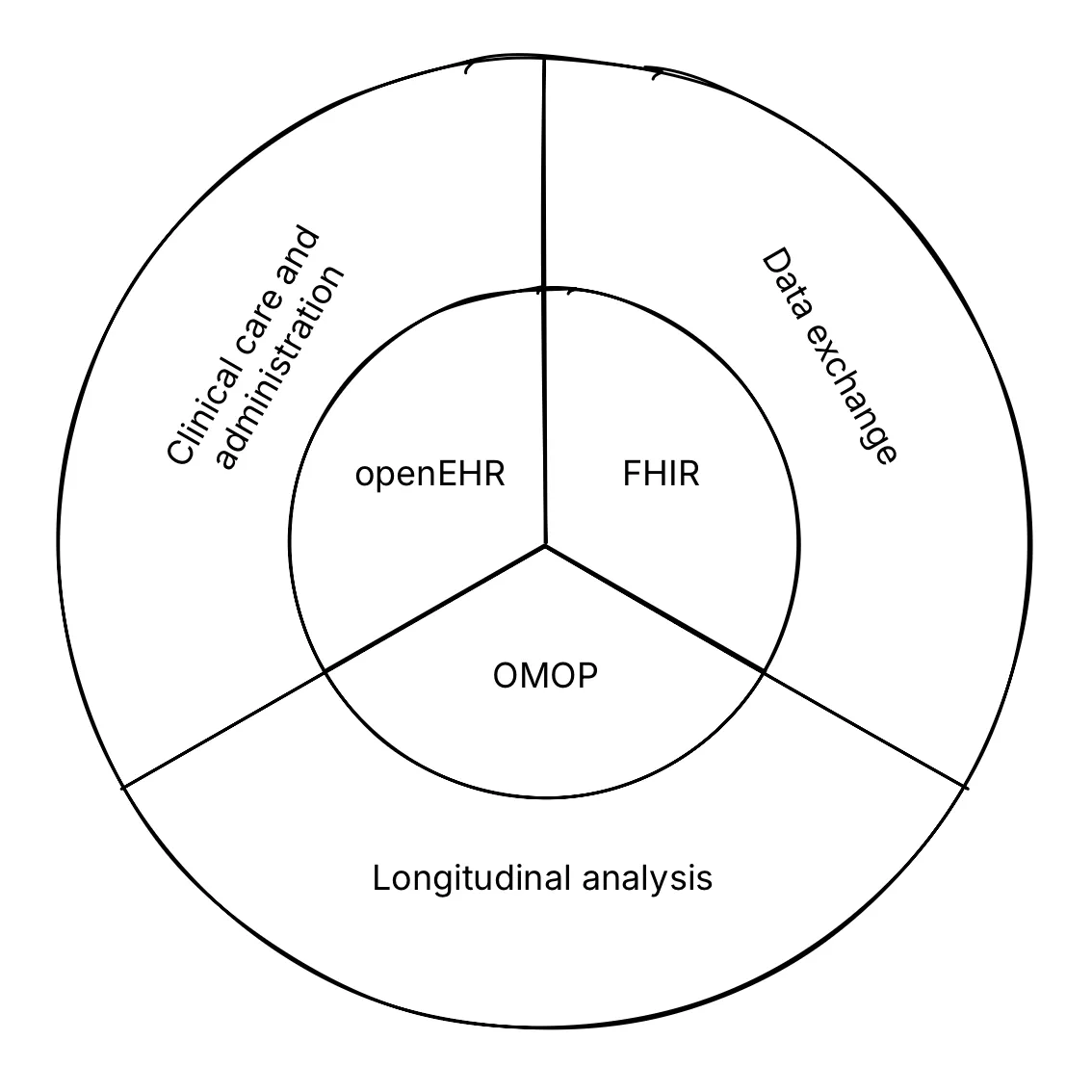
Using the example of Finland, Hanna discusses how different health data standards can coexist efficiently. Instead of competing, openEHR, FHIR, and OMOP each serve distinct roles within the country’s digital health ecosystem. In practice, openEHR is used as the core clinical data repository, FHIR as the data exchange layer, and OMOP supports secondary use cases such as research and analytics.
Finland’s regulatory and standards bodies are now working to strengthen alignment between these ecosystems. Hanna explains that the National Institute for Health and Welfare (THL) is leading efforts to use OMOP for national quality registries. HL7 Finland is a member of openEHR International and has established an openEHR modelling subgroup. Together, these initiatives ensure that FHIR, openEHR and OMOP remain complementary tools, not competing silos in building Finland’s interoperable health infrastructure.
A recent paper co-authored by leaders from the OMOP, openEHR, and FHIR communities proposes a shared framework for understanding how different health data standards serve distinct needs and priorities. The authors categorize these needs into 3 domains: Clinical Care and Administration, Longitudinal Analysis, and Data Exchange. The figure below shows how openEHR, FHIR, and OMOP align with these domains and offer complementary strengths.
The next phase of interoperability
Hanna says that the Nordic countries are still at the “baby steps” of interoperability, even with the widespread openEHR adoption. The next phase, as she puts it, is all about “mixing and matching”. Combining data, applications, and platform modules across different vendors and care settings is where real power lies.
This approach will move beyond the idea of a single, all-encompassing EHR, instead allowing regions to assemble technology ecosystems that best suit their needs. Hanna calls this the “best-of-breed” model, where modules from different suppliers, in-house developments, and niche applications can be combined to serve clinical requirements.
She also predicts a shift towards federated open platforms, where multiple openEHR-based and open-source systems can coexist. Data will increasingly flow from EHRs, devices, self-reported inputs, and wellness data. For Hanna, this marks the transition towards the adult phase of interoperability and creating connected and adaptive ecosystems.
openEHR education and awareness
Hanna’s journey as an educator began in 2020, when the COVID-19 pandemic pushed learning online. She launched an openEHR awareness course to make the topic accessible to a broader audience. “My customers said that openEHR is too difficult, too complex, and far too technical,” she recalls. Her goal was to create a course anyone could follow.
The program grew quickly, reaching participants in over 24 countries. Awareness and education are a key part of openEHR adoption, Hanna says, and essential to ensuring both vendors and hospital stakeholders are aligned. She also talks about empowering clinicians and decision-makers early in the process, in order to create believers who can drive the necessary cultural change within systems. For Hanna, education is the way to propagate the collaborative culture seen in the Nordic countries across the globe.
Quick recap
The Nordic journey shows that interoperability succeeds when collaboration is placed first, before competition or technology. A long-standing culture of data sharing between care systems created a strong foundation for the introduction of openEHR. Hanna Pohjonen shared insights on this ecosystem and how vendors drove openEHR adoption.
Finland demonstrates how openEHR, FHIR and OMOP are used together, serving distinct but complementary needs. Hanna notes that the next phase involves using federated ecosystems that connect multiple open platforms. For this evolution, education and awareness are critical, ensuring clinicians, decision makers, and vendors understand and champion the use of open, shared data.
Together, these elements form an example of what sustainable, national-level interoperability can look like in practice.
